A necessary step to healing the underlying wound tissue.
The word debridement stems from the French term ‘débridement’ which means ‘removing a blockage’. Debridement in wound care means the removal of dead (necrotic) and contaminated tissue in a wound [1]. It is therefore an important part of wound bed preparation. This article presents the positive effects of wound debridement on wound healing. Also, various debridement techniques are discussed as well as when these techniques are used.
Frequent debridement stimulates wound healing
Debridement improves tissue granulation (new tissue and blood vessels during healing process) and wound closure. Debrided wounds have a much better healing rate than wounds with necrotic tissue (dead tissue) [2].
Debriding chronic wounds to a point where healthy tissue is exposed, helps put the wound in an acute healing stage again, meaning that more growth factors, macrophages and keratinocytes rush to the wound bed [2].
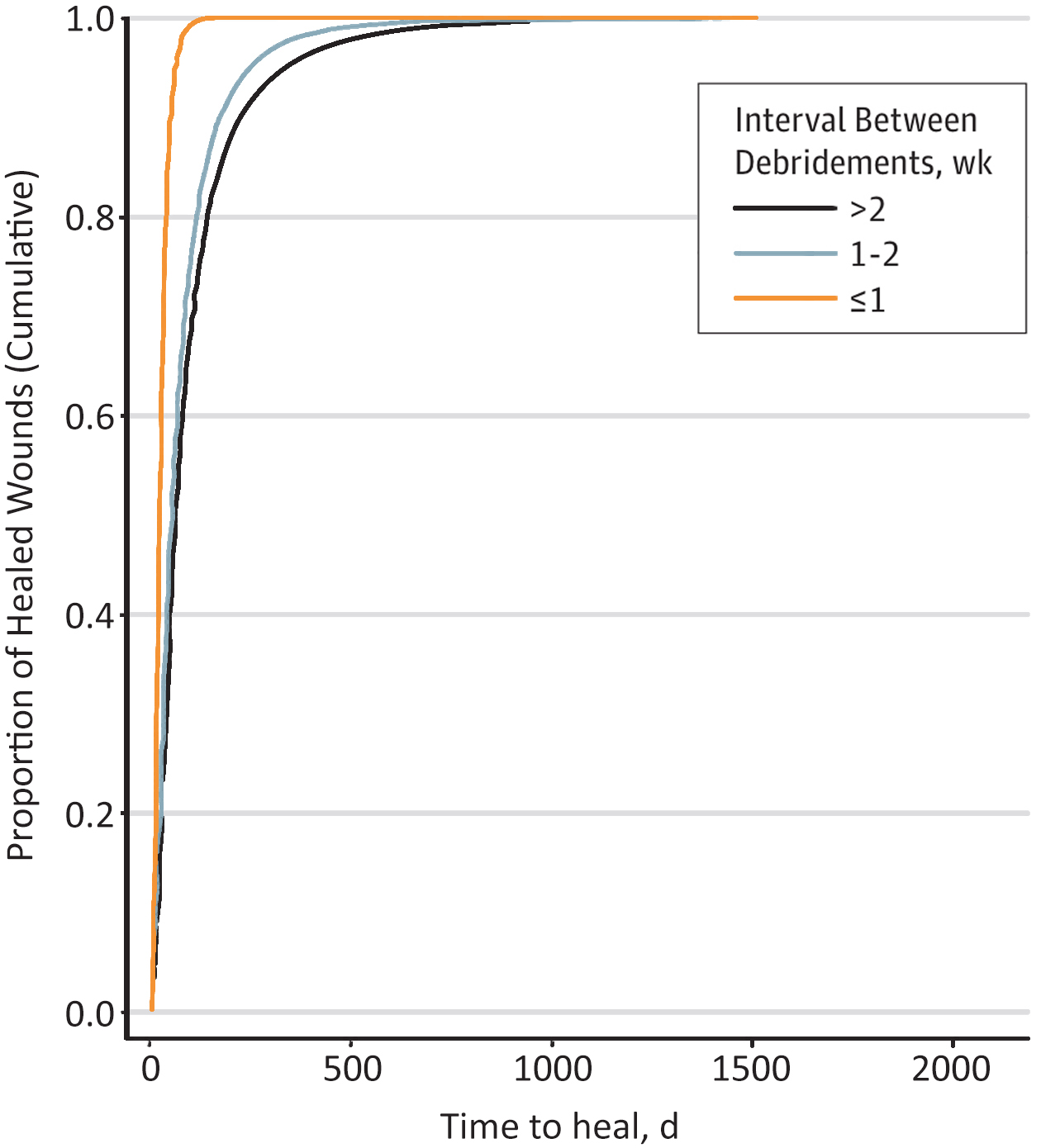
Graph 1: Shorter intervals between debridement of diabetic foot ulcers improve time to heal. [2]
If debridement is performed more than once a week (orange line), wounds heal faster. Wounds heal more slowly if debridement is performed less than once every 2 weeks (black line). [2]
How important is wound debridement?
Healing times were significantly faster in wounds where debriding was done more than once a week as evidence shows in study of more than 154,644 patients [2]. In contrast, wounds debrided less than every two weeks had a smaller likelihood of healing, and more than 70% of the wounds took more than 98 days to heal.
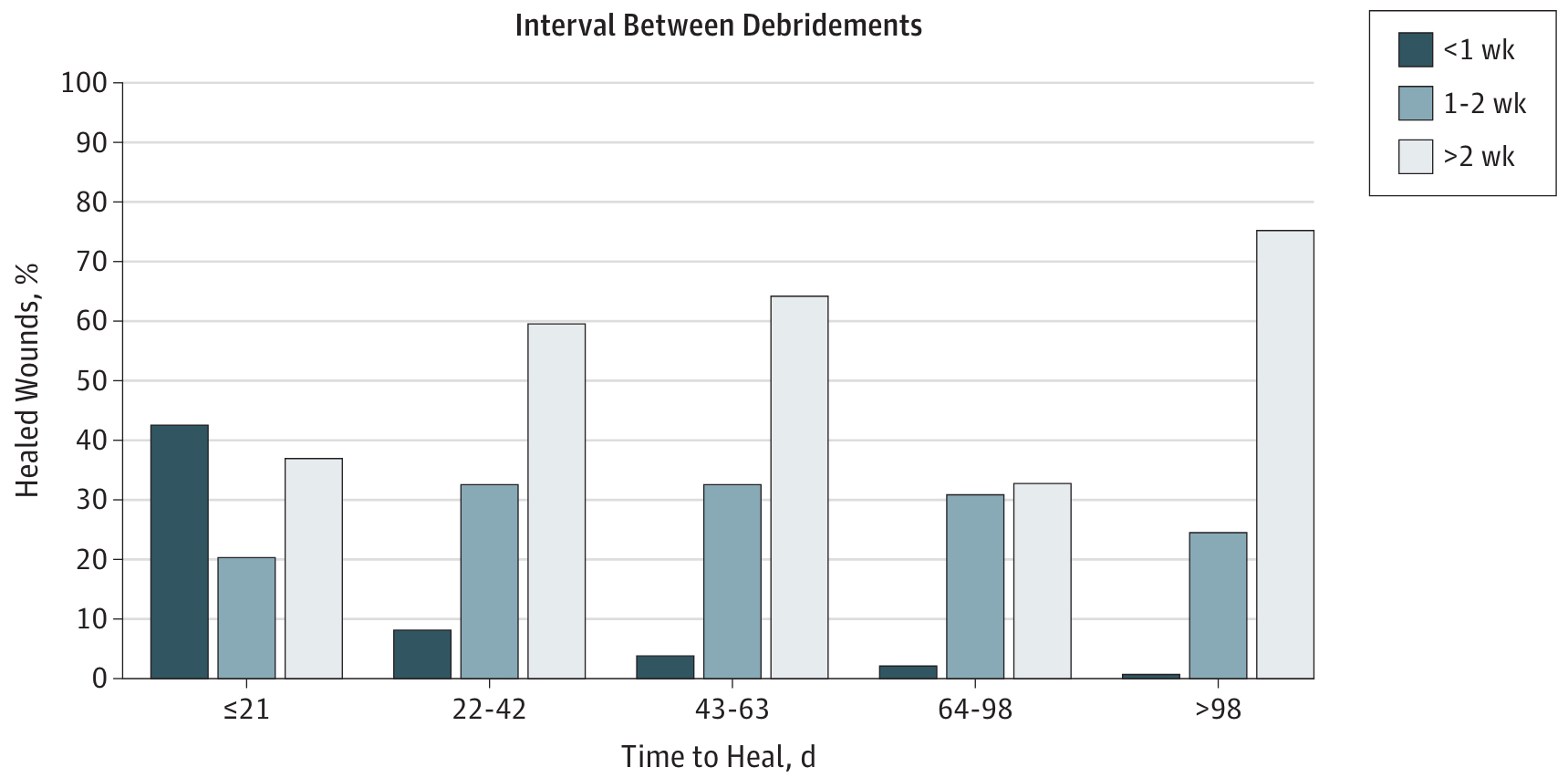
Graph 2: Association between percentages of healed wounds and time to heal.
“Wounds with a debridement interval of 1 week or less healed significantly faster.” [2]
The debridement method chosen should be effective in removing necrotic tissue and preventing the regrowth of biofilm [1] (the structure that protects bacteria and binds it to the wound surface [3]).
It is of the utmost importance that wound care nurses are comfortable with debridement and practice their wound debridement skills. When a trained wound care professional is not giving the care (such as diabetic foot care), patients should be referred to a certified wound care specialist.
Various debridement techniques
Widely used debridement techniques
Mechanical debridement
Mechanical debridement techniques in previous years involved the use of wet gauze being placed on the wound. The gauze dries while on the wound, sticking to the moisture from the wound. The gauze is then removed, along with the necrotic tissue covering the wound. This is called the ‘wet-to-dry’ method. It is still used today but may cause pain and bleeding. The materials are readily available, and the treatment is simple. [1]
A newer method is the use of microfibre pads. Dead tissue is lifted off the wound bed by sticking to the fibres in the pad. Microfibre pads cause less pain on the wound bed than the ‘wet-to-dry’ technique because you do not have to wait for the gauze to dry before removing the dead tissue.
Mechanical debridement is a great technique to use on wounds that are fragile, painful and bleed easily such as burn wounds, venous leg ulcers (ulcus cruris venosum) and arterial leg ulcers (ulcus cruris arteriosum).
Sharp debridement
Sharp debridement is the process of using a curette, scalpel, or scissor to remove necrotic tissue on the wound and calluses around the wound [1]. This technique is often used with good efficacy. It is a technique usually performed on diabetic foot ulcers and wounds with dry, hard tissue and calluses. This is usually done by an expert wound care practitioner.
Callus removal promotes healing. The hard skin puts pressure on the underlying tissue causing inflammation. Rolled wound edges need stimulation to epithelialize (grow protective tissue to cover the wound). Debriding the wound edges and the calluses will improve epithelialization and wound closure. [4]
Diabetic patients and people with a history of diabetic foot ulcers should be seen by a wound care practitioner even after their wound has healed. Doing regular foot care exams for people with a history of ulcers helps prevent new ulcers from developing [5]. Calluses and corns should be removed and monitored because the patient’s loss of protective sensation (neuropathy) puts him at risk for new wounds.
Autolytic debridement
Autolytic debridement makes use of wound moisture and the body’s own healing properties to debride the wound. Autolytic dressings facilitate a moist wound environment, softens necrosis and reduces bacterial load. The dressings may or may not contain antimicrobial properties [1].
Examples of autolytic debridement dressings include hydrofibres that turn into a gel-like texture when in contact with wound moisture. Hydrocolloids, hydrogels, and certain highly absorbent dressings also have autolytic properties [1].
This type of debridement works best for wounds that do not have an uncontrolled infection because infections can be aggravated by the warm, moist wound area.
Enzymatic debridement
Enzymes are particles that accelerate chemical processes such as breaking down proteins (in the case of wounds) and makes it easier to remove dead tissue [1]. Enzymatic debridement has greatly improved in the past few years. Many types of enzymes are available, including animal enzymes (krill), plant enzymes (papaya, pineapple [1] and bacterial enzymes (collagenase) to name a few [6].
Enzymatic debridement is useful in many kinds of wounds due to its antimicrobial properties as well as loosening necrosis. In wounds with a lot of dirt, necrotic tissue and moisture, enzymatic debridement can be a good option.
Biosurgical debridement
The secretions from larvae or maggots have antimicrobial properties. The way in which maggot therapy works is three-fold: debridement, antibacterial action and stimulation of healing. Their fast mode of action makes it a cost-effective treatment. A great benefit is that larvae can separate necrotic tissue from healthy tissue allowing easier surgical debridement afterwards [4].
A randomised controlled trial (one treatment group and one control group) investigated larval therapy for the debridement of venous leg ulcers [7]. In cases where patients reported the treatment to be uncomfortable or that they had experienced pain, the larval therapy did improve the appearance of the wound. If pain relief is well managed, patient education and treatment is done appropriately, debridement with larvae can be highly beneficial.
Surgical debridement
Surgical debridement is the process of surgically removing any unwanted dead tissue and even cutting into healthy tissue. During surgical debridement, a wound can be closed by primary (with stitches) or secondary (granulation and epithelialization) intention.
By cutting into healthy tissue, the wound is kickstarted to start healing. Macrophages, fibroblasts, keratinocytes, neutrophils and leukocytes will flood to the wound bed. Wounds that may benefit from surgical debridement include a pressure ulcer staging in stage 3 or 4, a diabetic foot ulcer, burn wounds and other necrotic wounds. Surgical debridement can effectively and quickly remove slough, necrosis, eschar, and dirt [1]. It is an essential procedure when the dead tissue becomes life-threatening for the patient. However, caution is needed for patients with many risk factors causing delayed wound healing since the wound will be enlarged by surgical debridement.
Debridement techniques based on newer technologies
Wound lavage systems
Jet lavage is a method of debridement using a fluid and pressure onto the wound bed to remove necrotic tissue. This method is effective and precise [1]. When using an antimicrobial fluid, microorganisms are destroyed as well.
Dissemination of particles into the air due to the force of the fluid may cause contamination of the treatment area or another part of the body. It is therefore important to prepare the surroundings to prevent contamination. The cost-efficacy of wound lavage systems relates to shorter hospital stays due to the precise and quick removal of infection-causing microorganisms [1]. Specific training and machinery is needed to perform this treatment.
Ultrasound debridement
Ultrasound / ultrasonic debridement means that sound waves are directed at the wound surface, causing a breakdown of biofilm and increasing microcirculation and granulation [4].
The user does need special training and specialised machinery to perform this treatment. This ultrasound technology is being used in specialised medical settings and for other healthcare applications, not only in wound care. This means that a wound care centre or larger care facilities may benefit from incorporating ultrasound machinery into their treatment regime.
Debridement is an important part of wound bed preparation
Adequate wound cleaning and debridement lay the groundwork to get the best outcome in wound healing. Debridement also plays a very important role in preparing the wound for advanced wound healing therapies such as hyperbaric oxygen therapy, negative pressure wound therapy (wound vac, vacuum assisted closure of a wound), skin grafts or cold plasma therapy. It is essential to make sure wound beds are kept clean and healthy and debrided frequently as this is directly related to the wound’s ability to heal.
What is your experience with debridement and how do you think it influences the results on wound healing in your wound care practice? Please post your reaction below.
A notification on new blogs will be posted in our newsletter. Below you can subscribe.
References:
[1] R. Strohal, J. Apelqvist and J. Dissemond. EWMA Document: Debridement. Journal of wound care, vol. 22, no. Suppl. 1, pp. S1-S52, 2013.
[2] J. R. Wilcox, M. J. Carter and S. Covington. Frequency of debridements and time to heal: A retrospective cohort study of 312744 wounds. JAMA Dermatology, pp. E1-E9, 2013.
[3] Britannica. www.britannica.com. The Editors of encyclopedia Britannica, 05 Feb 2009. [Online]. Available: https://www.britannica.com/science/biofilm. [Accessed 23 June 2021].
[4] C. Murphy, L. Atkin, T. Swanson, M. Tachi and Y. Tan. International Consensus document. Defying hard-to-heal wounds with an early antibiofilm intervention strategy. Journal of woundcare, vol. Suppl IIIb, no. 29, pp. 1-28, 2020.
[5] S. Khuraibet. Managing the diabetic foot ulcer [Webinar]. Urgo Medical, Qatar, 2020.
[6] B. V. Patry J.. Enzymatic debridement with collagenase in wounds and ulcers: a systematc review and meta-analysis. International wound journal, no. 14, pp. 1055-1065, 2017.
[7] E. Mudge, P. Price, N. Walkley and K. G. Harding. A randomised control trial of larval therapy for the debridement of leg ulcers: results of a multicenter, randomised, controlled, open, obsesrver blind, parallel group study. Wound repair and Regeration, no. 22, pp. 43-51, 2014.
These articles have been interpreted by people from Plasmacure BV. Questions related to this blog are answered by our wound experts. Mail to blog@plasmacure.nl


React